
My role
Sr. Product Designer
- Lead product strategy & design for the clinical product
- Lead planner and facilitator for presentations and working sessions for all clinical features
- Lead design researcher for interviews, and usability tests to solution workshops.
Timeframe
08/2023- 05/2024
(Research, design & implementation)
A phased-out approach was followed so we could validate our assumptions along the way.
Timeline breakdown here
Tools
- Figma
-
Miro
-
Illustrator
-
UserTesting.com
-
Looker
BACKGROUND
About Cerebral
Cerebral is a digital mental health company launched in January 2020 with strong growth. They mainly offer therapy and psychiatric video or phone visits for patients who are searching for accessible and convenient ways to access mental health care.

Project overview
The internal messaging tool is one of the most used functionalities in the application today. Patients use this tool to communicate with their clinicians and support teams outside of their video appointments when they have any questions, or concerns or just want to share their progress. These communications range from clinical questions, scheduling, billing, progress on goals, or any other topic of interest to the patient.
Overall the Messaging functionality at Cerebral has been continuously iterated over the last year as we learn more from continuous research.
In this case study I will discuss how we decided on the scope for the first few phases of updating our messaging functionality and what we plan next to get closer to the ideal state solution systematically.








MOTIVATION
Why invest time in improving messaging?
Retention was the name of the game for 2023. We had to ensure that we built a sustainable, continuously improving product that our patients actually enjoyed using. Based on the preliminary findings listed below, we were confident that messaging was the right area of focus.
10% of our active patients send at least 1 message per week, which meant that this impact was significant enough to prioritize in our roadmap.
DISCOVER - RESEARCH
Why was the messaging feature leading to churn?
From the preliminary data we gathered at this point, we knew that the messaging feature was leading to patient dissatisfaction and that long wait times were the leading cause for this. What we didn't know at the time was why this was happening and where the workflow was failing.
Research Goals
🎯
Define the major pain points for all user groups using the messaging system.
🎯
Identify why response times from internal teams are so delayed.
Research methodology
Understanding the problem
1. Interviews
-
Clinicians (n=10 - a mix of therapists, prescribers, and on-call prescribers)
-
Support staff (n=10)
-
Patients who have utilized the messaging system (n=8)
All interview data was synthesized using an abstraction ladder methodology to identify themes
2. Contextual inquiry
We observed Support staff members receive and triage incoming patient messages (n=5)
3. CSAT and eNPS scores
Deep-dive into client eNPS and CSAT scores and added commentary from email surveys sent out to provide feedback on the current messaging experience
4. Unmoderated usability testing
Unmoderated usability testing of the current messaging system (n=5)

So many interviews...
Synthesis

Abstraction ladder to determine themes
We collected all interview notes in miro stickies and used abstraction laddering to determine the main areas of improvement for patients, as well as internal staff members.

Here's what we found...
Our core users consist of: 1. Clinicians, 2. Support members & 3. Patients
What did the process look like today?

Core user pain points ❌
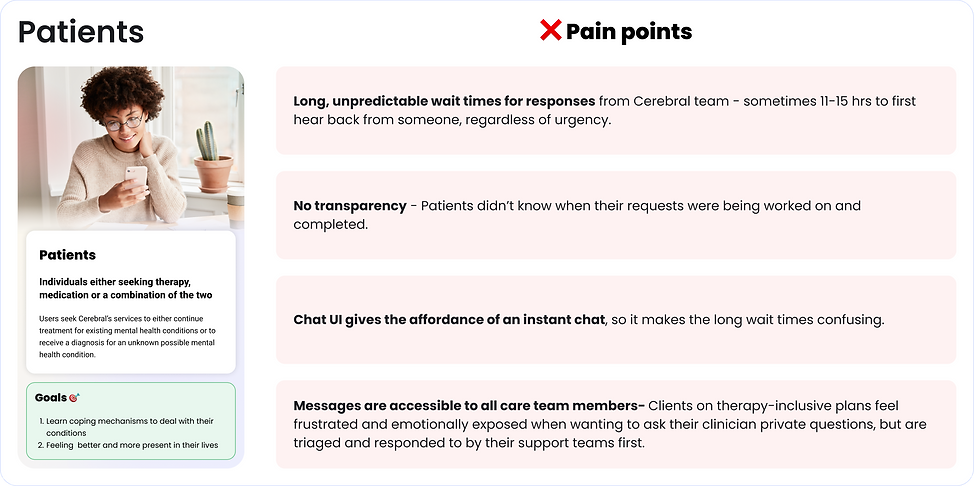


“I have no idea whether someone saw my message or not. I understand some of these things take time to sort out, but knowing whether they are even working on in the first place would be nice"
“The messaging system is absolutely terrible. I keep getting lost, it's glitchy as all get out and I keep having someone who isn't assigned to my care team answer my questions and frequently feel as though they didn't read the message before responding.”
“Communication with my care team looks easy with how many options there are for submitting contact, but getting a response couldn't be harder. I'm considering quitting over the shoddy communication I've experienced so far.”
“The only part I liked was my prescriber, who you laid off, and I now have one who won't even respond within A WEEK of me messaging her about important/urgent matters regarding my meds. The service is a joke. If I could afford an actual psychologist I would not be using Cerebral.”
DEFINE
Objectives
Based on all the pain points we had our jobs cut out for us. We narrowed it down to 4 main areas of focus below.
How might we deliver an effective communication solution that...
Improves operational efficiency and empowers teams to work at their highest potential?
Provides transparency and sets realistic expectations around resolution times?
Improves clinical quality by identifying and triaging messages appropriately based on urgency or content?
Guides users on their mental health journey, fostering trust, belonging, and support?
Ultimately, a task-based communication system that led to shortened resolution times for patient requests, that still felt personal and not transactional

Challenges
🧐
Creating a shared understanding between siloed teams and non-technical stakeholders
🧐
How to phase out the approach to not disrupt internal teams and confuse patients
🧐
Figuring out how task management and messaging meet in the middle
🧐
Ensure a task-based solution still feels personal and not transactional to patients
How did we overcome these challenges?
Solution o'clock
1. Brainstorming workshop
I conducted a brainstorming workshop including members of the R&D (Design, product & eng) as well as the clinical and operational teams.


2. ICE framework to prioritize features
We prioritized all the feature ideas using an ICE (Impact - Confidence - Effort) matrix.
3. Competitive analysis
We reviewed other mental health messaging services and non-mental health services that do a good job of keeping their messaging features clean and simple


4. Created a service blueprint
We created a service blueprint to showcase the new flows and better create a shared understanding between the involved teams. it turned out to be a great way for everyone to understand who is involved when.
DEVELOP
What we came up with...
* A messaging solution that would automatically create and triage tasks to the appropriate teams based on message content and urgency *
Patient → Internal team











Internal team → Patients




Internal system → Patient



Clients-side iterations after usability testing

From the operational side: Established on-call teams
The team model ensured that urgent messages and tasks were still resolved even when the assignees were out of office. An on-call prescriber and crisis team was established.
Examples of messages these teams picked up are:
-
Medication refills
-
Side effects
-
Crisis messages
-
Suicidal ideation

Data: RPA (robotic process automation) bots - We used machine learning to improve clinical quality
The data team built the CMD-1 tool using machine learning.
This tool identifies and shares messages from patients experiencing a mental health crisis with our crisis response specialists. It’s designed to alert the crisis response team to messages that may indicate suicidal ideation, homicidal ideation, non-suicidal self-injury, or domestic violence, among other emergencies. Once alerted, the crisis response team reaches out to patients directly to assess the level of immediate risk, then mobilizes emergency contacts and/or local responders, if appropriate.

The model successfully detected over 99% of all crisis messages and, as a result, crisis specialists were able to respond to patients in less than 9 minutes on average.
DELIVER
Outcomes: How did we do?
Reduced average resolution time by almost 80% (60hrs to 12hrs) for standard messages
Improved patient CSAT scores by 29% for wait times (60%-89%)
Improved clinical quality and safety by tracking and flagging messages with mentioned crisis situations
Achieved 80% CSAT score for new task system in the EMR
Timeline

Future iterations opportunities?


1. Create a more approachable and interactive experience to feel less static and more personal
2. Provide more robust resources for self-service resolutions, in cases where no urgency is required
3. Automate replies based on data within the client record if available and applicable (only 2% of messages are therapy-based, whereas 98% are admin related and resolution is within reach from a self-serve functionality)
